What Makes a Cell Responsive to a Particular Hormone?
The Endocrine Organisation
Hormones
Learning Objectives
Past the end of this department, you will exist able to:
- Identify the iii major classes of hormones on the basis of chemical structure
- Compare and contrast intracellular and cell membrane hormone receptors
- Draw signaling pathways that involve camp and IP3
- Identify several factors that influence a target jail cell's response
- Discuss the function of feedback loops and humoral, hormonal, and neural stimuli in hormone control
Although a given hormone may travel throughout the body in the bloodstream, information technology will affect the activeness only of its target cells; that is, cells with receptors for that detail hormone. Once the hormone binds to the receptor, a chain of events is initiated that leads to the target jail cell's response. Hormones play a critical function in the regulation of physiological processes considering of the target cell responses they regulate. These responses contribute to human reproduction, growth and development of body tissues, metabolism, fluid, and electrolyte residuum, sleep, and many other body functions. The major hormones of the homo trunk and their effects are identified in (Figure).
| Endocrine Glands and Their Major Hormones | |||
|---|---|---|---|
| Endocrine gland | Associated hormones | Chemical class | Effect |
| Pituitary (anterior) | Growth hormone (GH) | Protein | Promotes growth of torso tissues |
| Pituitary (anterior) | Prolactin (PRL) | Peptide | Promotes milk production |
| Pituitary (anterior) | Thyroid-stimulating hormone (TSH) | Glycoprotein | Stimulates thyroid hormone release |
| Pituitary (anterior) | Adrenocorticotropic hormone (ACTH) | Peptide | Stimulates hormone release by adrenal cortex |
| Pituitary (anterior) | Follicle-stimulating hormone (FSH) | Glycoprotein | Stimulates gamete production |
| Pituitary (anterior) | Luteinizing hormone (LH) | Glycoprotein | Stimulates androgen production by gonads |
| Pituitary (posterior) | Antidiuretic hormone (ADH) | Peptide | Stimulates h2o reabsorption past kidneys |
| Pituitary (posterior) | Oxytocin | Peptide | Stimulates uterine contractions during childbirth |
| Thyroid | Thyroxine (T4), triiodothyronine (Tthree) | Amine | Stimulate basal metabolic rate |
| Thyroid | Calcitonin | Peptide | Reduces blood Caii+ levels |
| Parathyroid | Parathyroid hormone (PTH) | Peptide | Increases blood Ca2+ levels |
| Adrenal (cortex) | Aldosterone | Steroid | Increases claret Na+ levels |
| Adrenal (cortex) | Cortisol, corticosterone, cortisone | Steroid | Increase blood glucose levels |
| Adrenal (medulla) | Epinephrine, norepinephrine | Amine | Stimulate fight-or-flight response |
| Pineal | Melatonin | Amine | Regulates sleep cycles |
| Pancreas | Insulin | Poly peptide | Reduces blood glucose levels |
| Pancreas | Glucagon | Protein | Increases blood glucose levels |
| Testes | Testosterone | Steroid | Stimulates development of male secondary sexual practice characteristics and sperm product |
| Ovaries | Estrogens and progesterone | Steroid | Stimulate evolution of female secondary sex characteristics and fix the body for childbirth |
Types of Hormones
The hormones of the human body can be divided into ii major groups on the footing of their chemic construction. Hormones derived from amino acids include amines, peptides, and proteins. Those derived from lipids include steroids ((Effigy)). These chemical groups touch on a hormone'southward distribution, the type of receptors it binds to, and other aspects of its function.
Amine, Peptide, Protein, and Steroid Hormone Construction
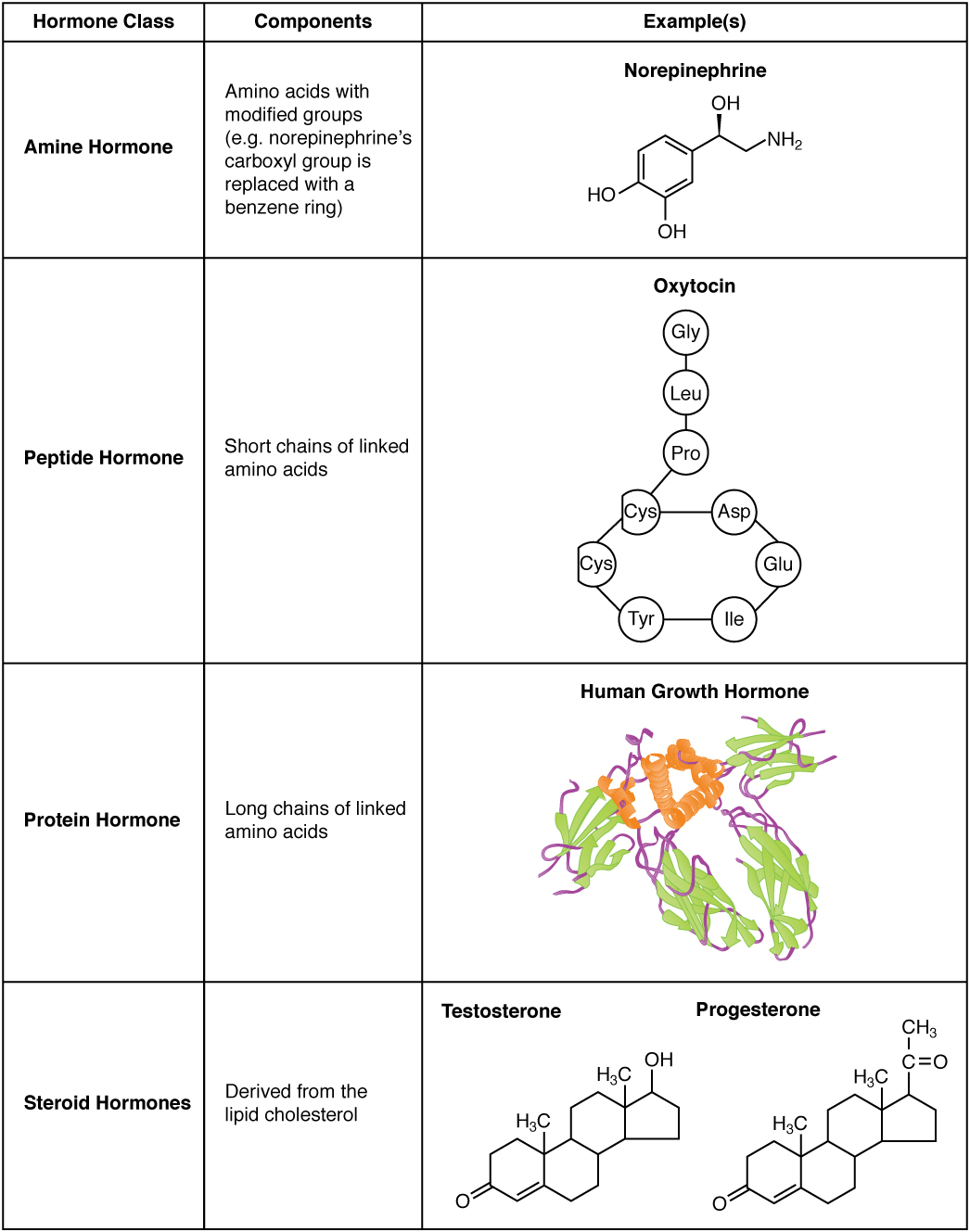
Amine Hormones
Hormones derived from the modification of amino acids are referred to every bit amine hormones. Typically, the original structure of the amino acid is modified such that a –COOH, or carboxyl, group is removed, whereas the [latex]-{\text{NH}}_{iii}^{+}[/latex], or amine, group remains.
Amine hormones are synthesized from the amino acids tryptophan or tyrosine. An example of a hormone derived from tryptophan is melatonin, which is secreted by the pineal gland and helps regulate circadian rhythm. Tyrosine derivatives include the metabolism-regulating thyroid hormones, also as the catecholamines, such as epinephrine, norepinephrine, and dopamine. Epinephrine and norepinephrine are secreted by the adrenal medulla and play a function in the fight-or-flight response, whereas dopamine is secreted by the hypothalamus and inhibits the release of sure anterior pituitary hormones.
Peptide and Protein Hormones
Whereas the amine hormones are derived from a unmarried amino acrid, peptide and protein hormones consist of multiple amino acids that link to form an amino acid concatenation. Peptide hormones consist of curt chains of amino acids, whereas protein hormones are longer polypeptides. Both types are synthesized like other body proteins: Deoxyribonucleic acid is transcribed into mRNA, which is translated into an amino acid chain.
Examples of peptide hormones include antidiuretic hormone (ADH), a pituitary hormone important in fluid rest, and atrial-natriuretic peptide, which is produced past the heart and helps to subtract blood pressure. Some examples of protein hormones include growth hormone, which is produced by the pituitary gland, and follicle-stimulating hormone (FSH), which has an attached carbohydrate group and is thus classified as a glycoprotein. FSH helps stimulate the maturation of eggs in the ovaries and sperm in the testes.
Steroid Hormones
The primary hormones derived from lipids are steroids. Steroid hormones are derived from the lipid cholesterol. For instance, the reproductive hormones testosterone and the estrogens—which are produced by the gonads (testes and ovaries)—are steroid hormones. The adrenal glands produce the steroid hormone aldosterone, which is involved in osmoregulation, and cortisol, which plays a role in metabolism.
Like cholesterol, steroid hormones are not soluble in water (they are hydrophobic). Because blood is h2o-based, lipid-derived hormones must travel to their target prison cell bound to a transport protein. This more circuitous structure extends the half-life of steroid hormones much longer than that of hormones derived from amino acids. A hormone'southward half-life is the time required for half the concentration of the hormone to be degraded. For case, the lipid-derived hormone cortisol has a half-life of approximately 60 to ninety minutes. In contrast, the amino acrid–derived hormone epinephrine has a half-life of approximately 1 minute.
Pathways of Hormone Action
The message a hormone sends is received by a hormone receptor, a poly peptide located either inside the cell or within the prison cell membrane. The receptor will process the message by initiating other signaling events or cellular mechanisms that issue in the target cell'south response. Hormone receptors recognize molecules with specific shapes and side groups, and respond only to those hormones that are recognized. The same type of receptor may be located on cells in different torso tissues, and trigger somewhat dissimilar responses. Thus, the response triggered past a hormone depends not only on the hormone, but also on the target prison cell.
Once the target prison cell receives the hormone signal, it tin can answer in a variety of ways. The response may include the stimulation of protein synthesis, activation or deactivation of enzymes, alteration in the permeability of the cell membrane, contradistinct rates of mitosis and prison cell growth, and stimulation of the secretion of products. Moreover, a unmarried hormone may be capable of inducing unlike responses in a given jail cell.
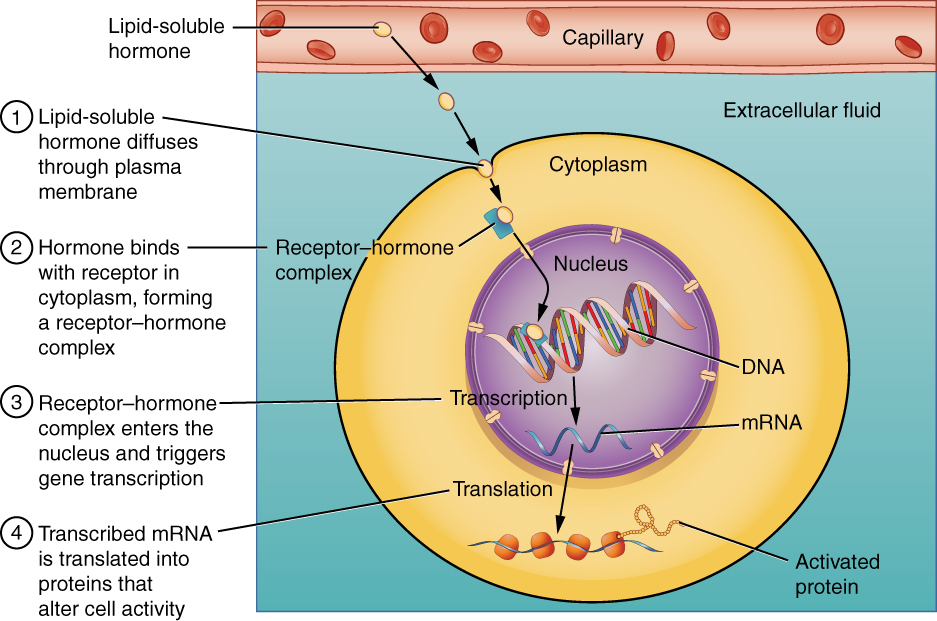
Pathways Involving Intracellular Hormone Receptors
Intracellular hormone receptors are located inside the cell. Hormones that bind to this type of receptor must exist able to cross the cell membrane. Steroid hormones are derived from cholesterol and therefore tin can readily diffuse through the lipid bilayer of the cell membrane to achieve the intracellular receptor ((Figure)). Thyroid hormones, which contain benzene rings studded with iodine, are also lipid-soluble and can enter the cell.
The location of steroid and thyroid hormone binding differs slightly: a steroid hormone may bind to its receptor within the cytosol or within the nucleus. In either instance, this binding generates a hormone-receptor complex that moves toward the chromatin in the jail cell nucleus and binds to a particular segment of the cell's Dna. In contrast, thyroid hormones bind to receptors already bound to DNA. For both steroid and thyroid hormones, binding of the hormone-receptor complex with Dna triggers transcription of a target gene to mRNA, which moves to the cytosol and directs protein synthesis past ribosomes.
Binding of Lipid-Soluble Hormones
A steroid hormone direct initiates the production of proteins within a target cell. Steroid hormones hands diffuse through the cell membrane. The hormone binds to its receptor in the cytosol, forming a receptor–hormone circuitous. The receptor–hormone complex then enters the nucleus and binds to the target gene on the Dna. Transcription of the cistron creates a messenger RNA that is translated into the desired poly peptide inside the cytoplasm.
Pathways Involving Prison cell Membrane Hormone Receptors
Hydrophilic, or water-soluble, hormones are unable to diffuse through the lipid bilayer of the cell membrane and must therefore pass on their bulletin to a receptor located at the surface of the cell. Except for thyroid hormones, which are lipid-soluble, all amino acrid–derived hormones bind to cell membrane receptors that are located, at least in part, on the extracellular surface of the jail cell membrane. Therefore, they practise non direct affect the transcription of target genes, simply instead initiate a signaling pour that is carried out past a molecule called a second messenger. In this case, the hormone is called a commencement messenger.
The 2nd messenger used by about hormones is cyclic adenosine monophosphate (cAMP). In the army camp second messenger organisation, a water-soluble hormone binds to its receptor in the cell membrane (Step 1 in (Effigy)). This receptor is associated with an intracellular component called a G protein, and binding of the hormone activates the G-poly peptide component (Step 2). The activated K protein in plow activates an enzyme called adenylyl cyclase, also known as adenylate cyclase (Step 3), which converts adenosine triphosphate (ATP) to cAMP (Step 4). As the second messenger, campsite activates a blazon of enzyme chosen a protein kinase that is present in the cytosol (Footstep 5). Activated protein kinases initiate a phosphorylation pour, in which multiple protein kinases phosphorylate (add a phosphate group to) numerous and various cellular proteins, including other enzymes (Step half-dozen).
Binding of Water-Soluble Hormones
Water-soluble hormones cannot diffuse through the cell membrane. These hormones must bind to a surface cell-membrane receptor. The receptor so initiates a cell-signaling pathway within the cell involving G proteins, adenylyl cyclase, the secondary messenger cyclic AMP (cAMP), and poly peptide kinases. In the final stride, these protein kinases phosphorylate proteins in the cytoplasm. This activates proteins in the cell that carry out the changes specified by the hormone.
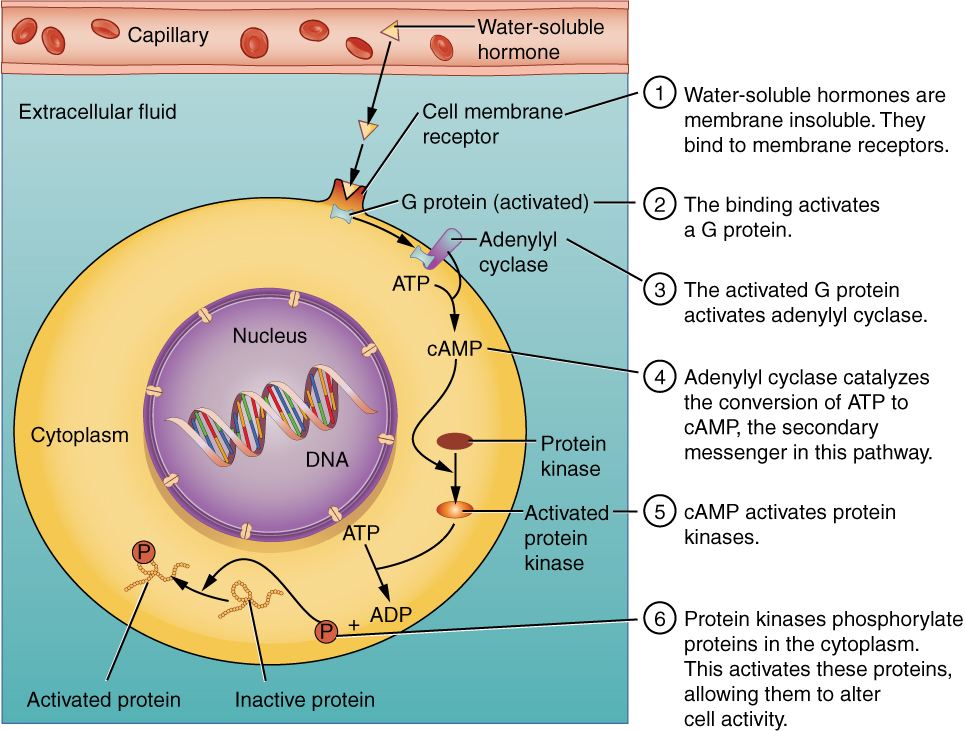
The phosphorylation of cellular proteins can trigger a wide variety of furnishings, from food metabolism to the synthesis of unlike hormones and other products. The effects vary according to the type of target prison cell, the G proteins and kinases involved, and the phosphorylation of proteins. Examples of hormones that employ cAMP equally a second messenger include calcitonin, which is important for bone construction and regulating blood calcium levels; glucagon, which plays a role in blood glucose levels; and thyroid-stimulating hormone, which causes the release of T3 and T4 from the thyroid gland.
Overall, the phosphorylation cascade significantly increases the efficiency, speed, and specificity of the hormonal response, as thousands of signaling events can be initiated simultaneously in response to a very low concentration of hormone in the bloodstream. However, the elapsing of the hormone point is brusque, equally camp is apace deactivated past the enzyme phosphodiesterase (PDE), which is located in the cytosol. The action of PDE helps to ensure that a target cell'south response ceases quickly unless new hormones arrive at the jail cell membrane.
Chiefly, in that location are also 1000 proteins that decrease the levels of military camp in the prison cell in response to hormone bounden. For example, when growth hormone–inhibiting hormone (GHIH), also known as somatostatin, binds to its receptors in the pituitary gland, the level of cAMP decreases, thereby inhibiting the secretion of homo growth hormone.
Not all water-soluble hormones initiate the campsite 2d messenger system. One common culling system uses calcium ions equally a 2d messenger. In this organisation, G proteins activate the enzyme phospholipase C (PLC), which functions similarly to adenylyl cyclase. Once activated, PLC cleaves a membrane-leap phospholipid into ii molecules: diacylglycerol (DAG) and inositol triphosphate (IP3). Like cAMP, DAG activates protein kinases that initiate a phosphorylation cascade. At the same time, IP3 causes calcium ions to be released from storage sites within the cytosol, such equally from within the smooth endoplasmic reticulum. The calcium ions then act equally second messengers in ii ways: they can influence enzymatic and other cellular activities straight, or they can demark to calcium-binding proteins, the most common of which is calmodulin. Upon binding calcium, calmodulin is able to attune protein kinase inside the jail cell. Examples of hormones that use calcium ions as a second messenger organisation include angiotensin Two, which helps regulate blood pressure through vasoconstriction, and growth hormone–releasing hormone (GHRH), which causes the pituitary gland to release growth hormones.
Factors Affecting Target Cell Response
You will recall that target cells must accept receptors specific to a given hormone if that hormone is to trigger a response. But several other factors influence the target cell response. For example, the presence of a pregnant level of a hormone circulating in the bloodstream tin cause its target cells to subtract their number of receptors for that hormone. This process is chosen downregulation, and it allows cells to become less reactive to the excessive hormone levels. When the level of a hormone is chronically reduced, target cells appoint in upregulation to increase their number of receptors. This process allows cells to be more sensitive to the hormone that is present. Cells can too alter the sensitivity of the receptors themselves to various hormones.
2 or more hormones tin interact to affect the response of cells in a variety of ways. The three about common types of interaction are as follows:
- The permissive event, in which the presence of one hormone enables some other hormone to act. For case, thyroid hormones have complex permissive relationships with certain reproductive hormones. A dietary deficiency of iodine, a component of thyroid hormones, can therefore touch on reproductive arrangement development and functioning.
- The synergistic effect, in which two hormones with similar furnishings produce an amplified response. In some cases, two hormones are required for an adequate response. For instance, ii dissimilar reproductive hormones—FSH from the pituitary gland and estrogens from the ovaries—are required for the maturation of female person ova (egg cells).
- The antagonistic effect, in which two hormones have opposing effects. A familiar example is the outcome of ii pancreatic hormones, insulin and glucagon. Insulin increases the liver'due south storage of glucose equally glycogen, decreasing blood glucose, whereas glucagon stimulates the breakdown of glycogen stores, increasing blood glucose.
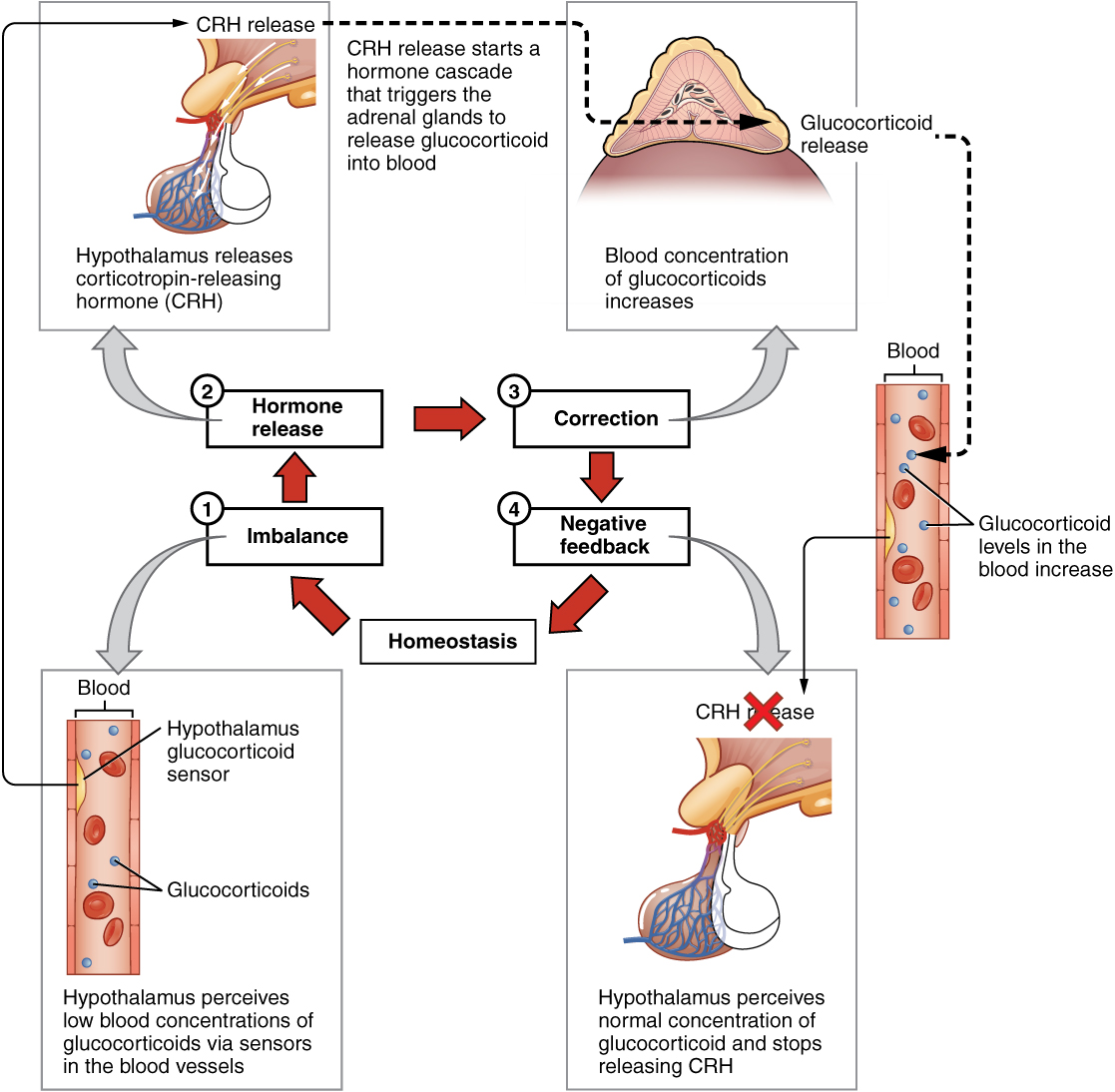
Regulation of Hormone Secretion
To prevent aberrant hormone levels and a potential illness country, hormone levels must exist tightly controlled. The torso maintains this control past balancing hormone product and deposition. Feedback loops govern the initiation and maintenance of nigh hormone secretion in response to diverse stimuli.
Role of Feedback Loops
The contribution of feedback loops to homeostasis will just be briefly reviewed here. Positive feedback loops are characterized by the release of additional hormone in response to an original hormone release. The release of oxytocin during childbirth is a positive feedback loop. The initial release of oxytocin begins to signal the uterine muscles to contract, which pushes the fetus toward the cervix, causing information technology to stretch. This, in turn, signals the pituitary gland to release more than oxytocin, causing labor contractions to intensify. The release of oxytocin decreases afterward the nativity of the child.
The more mutual method of hormone regulation is the negative feedback loop. Negative feedback is characterized by the inhibition of farther secretion of a hormone in response to adequate levels of that hormone. This allows blood levels of the hormone to exist regulated inside a narrow range. An instance of a negative feedback loop is the release of glucocorticoid hormones from the adrenal glands, as directed by the hypothalamus and pituitary gland. As glucocorticoid concentrations in the blood rising, the hypothalamus and pituitary gland reduce their signaling to the adrenal glands to forbid additional glucocorticoid secretion ((Figure)).
Negative Feedback Loop
The release of adrenal glucocorticoids is stimulated by the release of hormones from the hypothalamus and pituitary gland. This signaling is inhibited when glucocorticoid levels become elevated by causing negative signals to the pituitary gland and hypothalamus.
Function of Endocrine Gland Stimuli
Reflexes triggered by both chemic and neural stimuli command endocrine activity. These reflexes may be elementary, involving but one hormone response, or they may exist more than circuitous and involve many hormones, every bit is the case with the hypothalamic control of various anterior pituitary–controlled hormones.
Humoral stimuli are changes in blood levels of non-hormone chemicals, such as nutrients or ions, which cause the release or inhibition of a hormone to, in plough, maintain homeostasis. For example, osmoreceptors in the hypothalamus detect changes in claret osmolarity (the concentration of solutes in the claret plasma). If blood osmolarity is too high, meaning that the blood is non dilute plenty, osmoreceptors bespeak the hypothalamus to release ADH. The hormone causes the kidneys to reabsorb more than water and reduce the volume of urine produced. This reabsorption causes a reduction of the osmolarity of the blood, diluting the blood to the advisable level. The regulation of blood glucose is another example. High blood glucose levels cause the release of insulin from the pancreas, which increases glucose uptake by cells and liver storage of glucose as glycogen.
An endocrine gland may as well secrete a hormone in response to the presence of another hormone produced by a different endocrine gland. Such hormonal stimuli often involve the hypothalamus, which produces releasing and inhibiting hormones that control the secretion of a variety of pituitary hormones.
In addition to these chemical signals, hormones can also be released in response to neural stimuli. A common case of neural stimuli is the activation of the fight-or-flying response past the sympathetic nervous system. When an private perceives danger, sympathetic neurons bespeak the adrenal glands to secrete norepinephrine and epinephrine. The two hormones dilate blood vessels, increment the eye and respiratory rate, and suppress the digestive and allowed systems. These responses boost the trunk's transport of oxygen to the encephalon and muscles, thereby improving the body'south ability to fight or abscond.
Everyday Connections
Bisphenol A and Endocrine Disruption You may have heard news reports about the effects of a chemical called bisphenol A (BPA) in various types of food packaging. BPA is used in the manufacturing of difficult plastics and epoxy resins. Common food-related items that may incorporate BPA include the lining of aluminum cans, plastic food-storage containers, drinking cups, as well every bit baby bottles and "sippy" cups. Other uses of BPA include medical equipment, dental fillings, and the lining of water pipes.
Research suggests that BPA is an endocrine disruptor, pregnant that it negatively interferes with the endocrine system, specially during the prenatal and postnatal development period. In detail, BPA mimics the hormonal effects of estrogens and has the contrary effect—that of androgens. The U.S. Food and Drug Administration (FDA) notes in their statement almost BPA safety that although traditional toxicology studies have supported the safety of low levels of exposure to BPA, recent studies using novel approaches to test for subtle effects accept led to some concern about the potential furnishings of BPA on the brain, beliefs, and prostate gland in fetuses, infants, and young children. The FDA is currently facilitating decreased use of BPA in food-related materials. Many U.s. companies take voluntarily removed BPA from baby bottles, "sippy" cups, and the linings of infant formula cans, and virtually plastic reusable water bottles sold today boast that they are "BPA complimentary." In contrast, both Canada and the European Union have completely banned the employ of BPA in infant products.
The potential harmful effects of BPA have been studied in both brute models and humans and include a large diversity of health effects, such as developmental delay and disease. For instance, prenatal exposure to BPA during the first trimester of man pregnancy may be associated with wheezing and aggressive beliefs during childhood. Adults exposed to high levels of BPA may experience contradistinct thyroid signaling and male sexual dysfunction. BPA exposure during the prenatal or postnatal period of development in fauna models has been observed to cause neurological delays, changes in encephalon structure and office, sexual dysfunction, asthma, and increased risk for multiple cancers. In vitro studies have also shown that BPA exposure causes molecular changes that initiate the development of cancers of the breast, prostate, and brain. Although these studies accept implicated BPA in numerous ill health effects, some experts caution that some of these studies may be flawed and that more enquiry needs to be washed. In the concurrently, the FDA recommends that consumers take precautions to limit their exposure to BPA. In addition to purchasing foods in packaging gratis of BPA, consumers should avoid carrying or storing foods or liquids in bottles with the recycling lawmaking 3 or 7. Foods and liquids should not be microwave-heated in any form of plastic: utilize paper, glass, or ceramics instead.
Chapter Review
Hormones are derived from amino acids or lipids. Amine hormones originate from the amino acids tryptophan or tyrosine. Larger amino acrid hormones include peptides and protein hormones. Steroid hormones are derived from cholesterol.
Steroid hormones and thyroid hormone are lipid soluble. All other amino acid–derived hormones are h2o soluble. Hydrophobic hormones are able to diffuse through the membrane and interact with an intracellular receptor. In dissimilarity, hydrophilic hormones must interact with cell membrane receptors. These are typically associated with a G poly peptide, which becomes activated when the hormone binds the receptor. This initiates a signaling cascade that involves a second messenger, such every bit cyclic adenosine monophosphate (cAMP). Second messenger systems greatly amplify the hormone signal, creating a broader, more efficient, and faster response.
Hormones are released upon stimulation that is of either chemical or neural origin. Regulation of hormone release is primarily accomplished through negative feedback. Diverse stimuli may cause the release of hormones, merely there are iii major types. Humoral stimuli are changes in ion or nutrient levels in the blood. Hormonal stimuli are changes in hormone levels that initiate or inhibit the secretion of another hormone. Finally, a neural stimulus occurs when a nerve impulse prompts the secretion or inhibition of a hormone.
Review Questions
A newly developed pesticide has been observed to bind to an intracellular hormone receptor. If ingested, residual from this pesticide could disrupt levels of ________.
- melatonin
- thyroid hormone
- growth hormone
- insulin
B
A pocket-size molecule binds to a G protein, preventing its activation. What directly upshot will this have on signaling that involves cAMP?
- The hormone will non be able to demark to the hormone receptor.
- Adenylyl cyclase volition not be activated.
- Excessive quantities of military camp will exist produced.
- The phosphorylation cascade volition be initiated.
B
A student is in a motorcar accident, and although non injure, immediately experiences pupil dilation, increased heart rate, and rapid breathing. What blazon of endocrine system stimulus did the student receive?
- humoral
- hormonal
- neural
- positive feedback
C
Critical Thinking Questions
Compare and contrast the signaling events involved with the second messengers cAMP and IP3.
In both cAMP and IP3–calcium signaling, a hormone binds to a cell membrane hormone receptor that is coupled to a G protein. The G protein becomes activated when the hormone binds. In the case of cAMP signaling, the activated G poly peptide activates adenylyl cyclase, which causes ATP to be converted to army camp. This 2d messenger can then initiate other signaling events, such every bit a phosphorylation cascade. In the case of IPiii–calcium signaling, the activated 1000 protein activates phospholipase C, which cleaves a membrane phospholipid compound into DAG and IP3. IP3 causes the release of calcium, another second messenger, from intracellular stores. This causes further signaling events.
Depict the mechanism of hormone response resulting from the bounden of a hormone with an intracellular receptor.
An intracellular hormone receptor is located within the jail cell. A hydrophobic hormone diffuses through the jail cell membrane and binds to the intracellular hormone receptor, which may be in the cytosol or in the prison cell nucleus. This hormone–receptor circuitous binds to a segment of Dna. This initiates the transcription of a target gene, the finish result of which is protein assembly and the hormonal response.
Glossary
- adenylyl cyclase
- membrane-bound enzyme that converts ATP to cyclic AMP, creating cAMP, as a result of Thou-poly peptide activation
- cyclic adenosine monophosphate (army camp)
- second messenger that, in response to adenylyl cyclase activation, triggers a phosphorylation cascade
- diacylglycerol (DAG)
- molecule that, like cAMP, activates protein kinases, thereby initiating a phosphorylation cascade
- downregulation
- decrease in the number of hormone receptors, typically in response to chronically excessive levels of a hormone
- commencement messenger
- hormone that binds to a cell membrane hormone receptor and triggers activation of a second messenger system
- M protein
- protein associated with a cell membrane hormone receptor that initiates the next pace in a second messenger system upon activation by hormone–receptor binding
- hormone receptor
- protein within a jail cell or on the cell membrane that binds a hormone, initiating the target cell response
- inositol triphosphate (IPiii)
- molecule that initiates the release of calcium ions from intracellular stores
- phosphodiesterase (PDE)
- cytosolic enzyme that deactivates and degrades cAMP
- phosphorylation pour
- signaling outcome in which multiple protein kinases phosphorylate the next protein substrate by transferring a phosphate group from ATP to the protein
- poly peptide kinase
- enzyme that initiates a phosphorylation cascade upon activation
- second messenger
- molecule that initiates a signaling cascade in response to hormone binding on a cell membrane receptor and activation of a G poly peptide
- upregulation
- increment in the number of hormone receptors, typically in response to chronically reduced levels of a hormone
lombardibothe1936.blogspot.com
Source: https://opentextbc.ca/anatomyandphysiologyopenstax/chapter/hormones/
0 Response to "What Makes a Cell Responsive to a Particular Hormone?"
Post a Comment